How it all began…
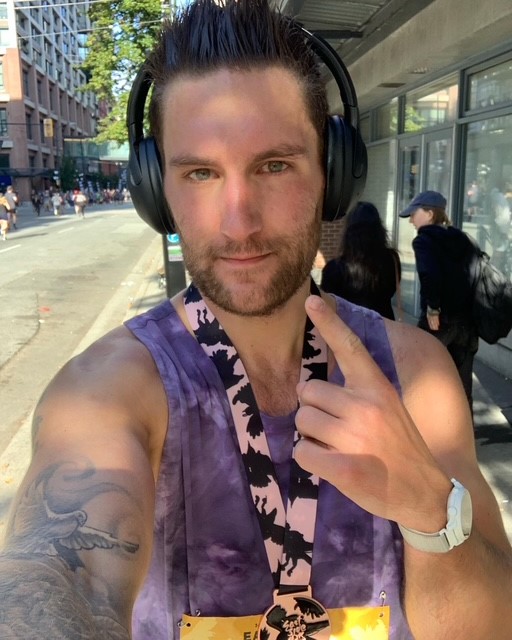
I was training for the Vancouver BMO Marathon scheduled for May 1st, 2023. As part of my preparation, I had also registered for and completed an earlier race—the Under Armour Eastside 10K, which took place on September 17th, 2022.
I was avidly running every single day in anticipation of both races. Not long after completing the 10K in September 2022, I started experiencing unusual symptoms. Initially, I thought I was simply overtraining. The headaches were mild, sporadic, and manageable. Then came episodes of blurry and double vision, along with intermittent ringing in my ears (tinnitus). It wasn’t until I stepped onto a treadmill at the gym that I realized something was seriously wrong. With each stride, I felt immense pressure in my head. I told myself I just needed a rest day and continued trying every day for the rest of the week—but the symptoms didn’t go away.
As the headaches became more frequent and increasingly severe, I began to suspect something more serious—possibly a brain tumor. I voiced these concerns to friends and family, but they dismissed them, calling me a hypochondriac. Around this time, I also began to notice changes in my behavior: I was more irritable and aggressive in conversations, which, unbeknownst to me, is a symptom of GBM (Glioblastoma).
On the morning of October 28th, 2022, I felt worse than ever. I began my usual morning routine with a hot shower, but dizziness, nausea, and a total loss of equilibrium hit me like a brick. It felt like I was dying. With the cumulative symptoms and this intense episode, I knew it was time for immediate action. I had already spent weeks researching potential causes and had ruled out nearly everything—except a brain tumor.
During my research, I discovered that an eye exam could be an effective and affordable first step in identifying brain issues. With MRIs taking months unless done privately (at a cost of $800), I opted for a $100 eye exam—thankfully only $20 for me due to extended health benefits. I called the optometrist immediately after the shower incident and got an appointment that afternoon. After explaining my symptoms, the exam revealed that my optic nerve was extremely swollen and bleeding due to pressure. I was urgently sent to Surrey Memorial Hospital for further testing.
At the hospital, I was told there would be a short wait before I could get a CT scan. My wife joined me, and once the scan results were in, we received the heartbreaking diagnosis. She couldn’t stomach the news and broke down in tears. It was Friday, October 28th, and I was told I would need brain surgery (resection) the following Monday—November 1st, 2022. The tumor was described as being the size of a peach. I was extremely lucky to have no speech impediment given the tumor’s size and location.
Everything moved quickly. I met with the neurosurgeon who would be operating on me and was briefed on the procedure and possible complications. Prior to the biopsy, it was suspected to be a grade 2 tumor, which would have been preferable due to its slower growth rate. Emotionally overwhelmed, I struggled to absorb all the information being thrown at me.
Surgery came and went on November 1st. When I woke up, I was ecstatic to be alive. The surgeon had successfully removed 60–70% of the tumor. It was located in my occipital lobe, and any further removal risked blindness or death. The extracted tissue was sent to Vancouver General Hospital for analysis. The pathology report confirmed the worst: it was Glioblastoma, a grade 4 brain tumor—one of the most aggressive and incurable cancers, with a 100% chance of recurrence. I was given a prognosis of 12–18 months to live.
This news was devastating. I turned to my radiologist and said, “I’ll see you in two years for a follow-up,” to which he smirked and replied, “No you won’t.” But I wasn’t just making a bold statement—I genuinely believed it. Two weeks before my diagnosis, I had listened to Episode 78 of the Loosely Enlightened podcast featuring “Lee Whitley – The Man Who’s Curing Cancer.”[Listen Here] It resonated deeply with me and planted a seed that would soon become my lifeline.
I’m not religious, but I consider myself spiritual. I saw this as an opportunity I couldn’t afford to ignore—I had nothing to lose. By then, I was bedridden and extremely sick. Thankfully, my wife reached out to Lee and his wife, and I began taking his cancer support medication on November 14th, 2022. [View Table 1.1 on the Events/Timeline Page.]
It was a difficult decision. There weren’t many testimonials back then about Lee’s treatment, and I was terrified. Oncologists and hospital staff instilled a sense of urgency and fear in me. Still, I resolved to do everything I could to fight this disease. I decided to pursue both conventional (Standard of Care, SOC) and alternative treatments. Either Lee Whitley was 100% sincere, or he was the biggest fraud alive. I’m relieved to say I made the right choice. Every MRI since has shown nothing but tumor shrinkage, and by October 2024, I was declared in remission—no signs or symptoms of disease.
Next, I’ll dive into the standard of care treatment I underwent, which involved a combination of chemotherapy (TMZ) and radiation. [View Table 1.1 on the Events/Timeline Page.]
SOC Treatment



Let me start by saying it wasn’t always rainbows and butterflies. I already mentioned previously that getting a cancer diagnosis is a deeply emotional process for everyone involved—not just the patient, but everyone around them. I decided to undergo chemo and radiation because I believed it would help me survive. My will to live was enormous. Like I said, I wanted to do everything and anything that would give me even a 0.01% chance of survival.
Knowing what I know now, I would have never done the standard of care (SOC) treatment. I actually refused it when it was offered to me again, because I had no reason to continue—it never recurred, and my tumor never stopped shrinking. I always feared that chemo and radiation would cause irreversible long-term damage, and that fear wasn’t unfounded. After all, chemotherapy was derived from mustard gas during WWII.
At the start of treatment, I was getting MRIs every two months, which later became every three months once I started doing well. I also had a herniated disc from a workplace injury prior to my cancer diagnosis. It was left untreated because my employer denied it had happened on the job—for reasons I won’t get into. That injury worsened over time and developed into degenerative disc disease. It pressed on my nerves constantly, causing radiating pain, numbness, and tingling down my leg.
Sadly, just when you think things can’t get worse—they can. I experienced a level of pain I would rate as 10/10 for months, even years. Part of it was due to my back injury, but I also developed chronic neuropathic pain from my brain operation. The pain was unbearable, even for someone like me who considers themselves mentally and physically tough with a high pain threshold. I brought this up to several doctors. The pain was widespread—so much so that a nurse suggested I might have fibromyalgia, and my family doctor thought I had hip bursitis.
But the pain didn’t let up. It intensified, and eventually, I developed a burning sensation in my leg that never went away. It got so bad I couldn’t walk properly for six months—I was literally crawling on the floor of my house. Every time I saw my oncologist, I mentioned it. I insisted I had a blood clot for six months, and each time he said, “I don’t think it’s a blood clot; you’re not presenting with symptoms.”
What’s important to understand is that even though I looked fine on the outside—physically healthy—I was very sick, extremely lethargic, and suffering immensely. Eventually, I collapsed in my bedroom while talking to my wife. I could barely breathe and managed to crawl close enough to a fan to get some air. I felt like I was suffocating. My wife asked if I needed to go to the hospital, but I refused—probably because of the same stubbornness that’s kept me alive this long.
It turned out I was right. It was a blood clot—a massive pulmonary embolism that nearly killed me. After that, I was referred to a hematologist who informed me I’d be on blood thinners for life, since GBM patients are prone to clots. The tumor creates artificial arteries to feed itself, but they’re fragile and break easily. I was prescribed heparin, an injectable blood thinner, which I had to take twice a day.
Let me tell you—heparin injections are brutal. They cause internal bruising every time, and when the medication goes in, it burns like fire. After three months of doing this twice daily, I broke. I told the doctor I’d rather die than continue. He switched me to an oral blood thinner, which didn’t have much data on GBM patients, but I didn’t care—anything was better.
At this point, I was on my deathbed. I was drained. Nothing was going right. I had debilitating side effects from chemo and radiation that lasted for months and even years—chemo brain, dizziness, jaundiced skin. My chemo cycle was postponed because my blood levels dropped too low. My red blood cells had crashed. I was diagnosed with hemolytic anemia and was on the verge of needing a transfusion.
This was the turning point in my journey. I genuinely didn’t think I had much time left. My initial prognosis was 12–18 months, which was later extended to 3 years due to a favorable IDH mutation. The bad luck just kept piling up—but so did the hidden blessings, like hearing that life-changing podcast just two weeks before my diagnosis. I truly believe mindset plays a major role in surviving cancer, and I made it a point to always stay focused on the positives.
Then, I received a call out of the blue from a neurosurgeon who had been following up about my herniated disc. I had so many doctors on my “cancer team” that I was confused about who he even was at first. But then he said, “A lot has happened since we last spoke. Do you know how much of your tumor was removed during surgery?” I told him 60–70%, and he told me he wanted to operate again—because the industry standard is 95%+.
I was stunned by his confidence. Honestly, he was cocky. When I asked why he thought he could do more than my original surgeon, he said, “I did five brain operations before lunch yesterday.” He warned me I might lose vision in my left eye, but said the operation would likely add years to my life—beyond the 3 years I had been given.
My radiologist and oncologist were completely against it. They said my first surgeon had good reasons not to go further. But I didn’t listen. My stubbornness had gotten me this far—I was betting my life on this new surgeon. On May 3, 2023, I had my second brain resection. I met him in person for the first time about 5–10 minutes before surgery. He warned me again—he was confident I’d lose full vision in my left eye and probably never drive again.
But my decision was final: life over limb. I just wanted more time with my wife, son, and family.
Well, I’m happy to report that I woke up alive—and not only that, he successfully removed over 95% of the tumor, and I didn’t lose full vision. The swelling eventually subsided, and a vision test showed I had only minimal peripheral loss in my left eye—and I was legal to drive!
Things only improved from that point. But I’ll never forget how close I came to death. I consider myself extremely lucky. Even now, doctors say GBM has a 100% recurrence rate, but I’m healthier now than I was before the diagnosis. The combination of SOC and alternative treatments worked for me.
That said, I strongly advise against chemo and radiation for others. They aren’t a cure and come with dangerous side effects—like osteopenia, which I developed. These treatments can even cause your cancer to metastasize. And once you do SOC, it becomes much harder to heal using alternative approaches. That’s why I’m so passionate about helping other cancer patients who are facing similar decisions.
From the very beginning, I had a gut feeling things would be okay. During my first meeting with the radiologist, he asked what vitamins or supplements I was taking. I rattled off a list of 20. When I said the last one—Full-Spectrum CBD oil—he turned his head quickly and asked, “Who told you to take that?” I replied, “I did my own research.” That moment told me I was on the right path.
So if you’re going through a cancer diagnosis or something similar, my advice is: accept the diagnosis, not the prognosis. Listen to your doctors, but also take time to dissect the information with your family. Do it in a relaxed state, so your decision comes from logic, not fear—or external pressure.
Whatever diagnosis you receive, remember—nothing catastrophic is going to happen in the next 24 hours. You have time. You have options. And above all: Don’t panic, call Lee.

Audio Recording-Oncologist
My oncologist and I discussing the alternative treatment (Lees Oils) and his positive feedback.